A Simple Guide to Vasectomy Medical Term and Procedure
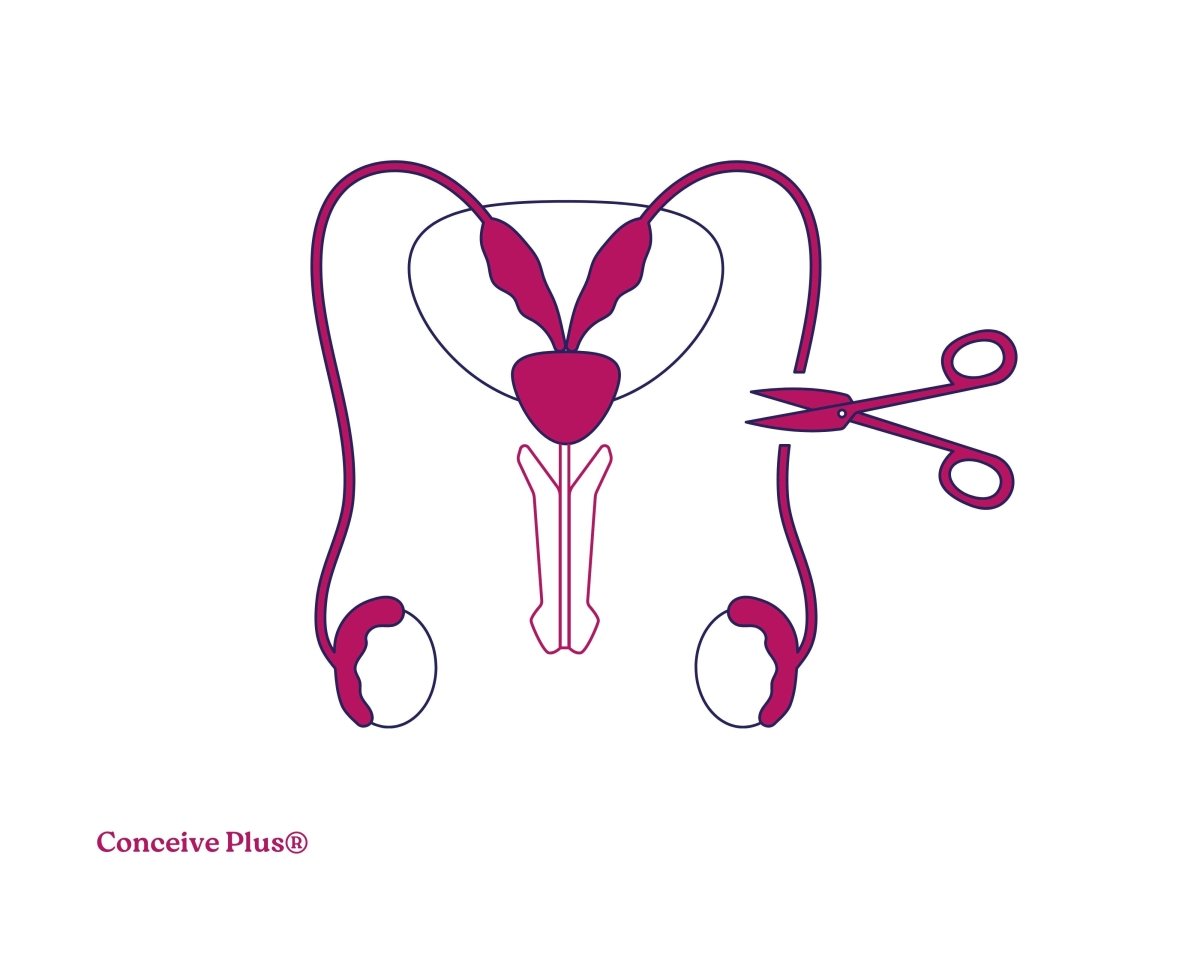
A vasectomy is a surgical procedure that provides permanent contraception. In this procedure, the sperm-carrying tubes from the testicles are cut, blocked, or sealed [1].
A male can still get an erection and ejaculate semen after the vasectomy surgery [2]. This surgery just prevents sperm from mixing with semen. Those men go for this procedure who no longer want to have children and want a permanent and reliable birth control option.
The vasectomy procedure is considered a safe and effective contraception method, offering permanent results without affecting sexual performance or sexual experience. This article explains the vasectomy medical terms and procedure for those looking for a permanent contraception option.
Who Needs a Vasectomy?
Men who decide that they do not want to have more children or any at all typically choose a tied testicle or vasectomy procedure for birth control. This male surgical contraception method is common among men who have children and are sure they do not want to expand their families.
In some cases, vasectomy may be recommended for men who have certain genetic conditions and do not wish to pass those abnormalities on to future generations [3].
As it is a permanent procedure, it is important to make up your mind and be confident about your decision of not wanting to expand the family in the future.
Medical Terms Involved in Vasectomy
Information about male body anatomy and different medical terminologies involved in the vasectomy procedure can help you better understand how this contraception method works.
The list of medical terms involved includes:
- Vasectomy: The overall surgical procedure for cutting or blocking the sperm-carrying tube is medically known as vasectomy.
- Vas Deferens: These are the tubes that carry sperm from the testicles to the urethra [4]. In a vasectomy, these tubes are cut or sealed, preventing sperm from entering the semen.
- Spermatic Cord: The spermatic cord is a bundle of blood vessels, nerves, and the vas deferens [5]. The surgeon looks for the vas deferens through the spermatic cord during vasectomy.
- Local Anesthesia: Local anesthesia is typically used during vasectomy to make the procedure painless for the patient. This procedure numbs the area to be operated.
- Cauterization: It is the process of killing the desired tissues using chemicals or extreme temperatures [6]. It is used in vasectomy to seal the vas deferens — the tube that carries sperm.
Process Involved in Vasectomy
The complete vasectomy can be divided into simpler steps for better understanding. The steps involve:
-
Preparation
Before the procedure, the doctor will explain the process to you in detail so that you can make an informed decision. If you agree to the surgery, the procedure starts with applying local anesthesia to numb the area.
-
Incision or No-Scalpel Method
In the traditional vasectomy, small incisions are made on either side of the scrotum — outer skin pouch holding testes — to access the vas deferens.
Besides the traditional method, a modern no-scalpel method is also common. In the no-scalpel method, a surgeon makes a small puncture instead of a cut, significantly reducing the risk of complications.
-
Sealing the Vas Deferens
Once the doctor accesses the vas deferens, they are cut. After the cut, the two ends are either tied, cauterized, or sealed to prevent sperm from reaching the semen.
-
Closing the Incisions
After the vas deferens are sealed, the small incisions are closed with stitches or allowed to heal naturally. The time it takes for the wound to heal will depend on multiple factors, including post-operative care.
Vasectomy Recovery
The patient usually recovers from vasectomy quickly. You shouldn't be stressed if you experience mild discomfort, pain and swelling, or bruising for a few days after the procedure.
Ice packs and over-the-counter pain relievers can help manage post-operative symptoms. Most men can return to work within a few days, but you need to avoid heavy lifting or activities that put stress on the testes.
You can also resume sexual activity typically after about a week. It is recommended to use protection until a follow-up sperm test confirms the absence of sperm in the semen. If you are having second thoughts about becoming a daddy after vasectomy, you should know what are the 5 stages of IVF, an assisted way to become a father.
The Bottom Line
Vasectomy is a highly effective male fertility operation for men who want a permanent birth control solution. It is a male surgical procedure where the sperm-carrying tube is cut and blocked. The vasectomy medical term refers specifically to the surgical interruption of the vas deferens to achieve male sterilization.
Tied testicles prevent the entry of sperm cells into the semen, preventing pregnancies. A man can engage in sexual activities even after vasectomy and can ejaculate semen without sperm cells.
The ejaculation after vasectomy can't fertilize an egg and cause conception, which is the goal of this treatment procedure.
FAQs
-
Can I reverse a vasectomy?
In most cases, vasectomy can be reversed with a small surgery where the sperm-carrying tube is connected again.
-
How to make yourself infertile?
Vasectomy is an example of a contraception method that can make you infertile permanently until you go for vasectomy reverse surgery.
-
Are there any side effects of vasectomy?
Vasectomy is mostly a safe procedure, and in rare cases, you can expect side effects. Normally, you can expect mild testicular pain from this surgery.
Resources Used
- Stormont, G., & Deibert, C. M. (2023, April 10). Vasectomy. StatPearls - NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK549904/
- Engl, T., Hallmen, S., Beecken, D., Rubenwolf, P., Gerharz, W., & Vallo, S. (2017). Impact of vasectomy on the sexual satisfaction of couples: Experience from a specialized clinic. Central European Journal of Urology, 70(3), 275-279. https://doi.org/10.5173/ceju.2017.1294
- Alliance, G. (2009, July 8). INHERITANCE PATTERNS. Understanding Genetics - NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK115561/
- Koslov, D. S., & Andersson, E. (2013). Physiological and pharmacological aspects of the vas deferens—An update. Frontiers in Pharmacology, 4. https://doi.org/10.3389/fphar.2013.00101
- Ramírez-González, J. A., & Sansone, A. (2021). Male reproductive system. Fertility, Pregnancy, and Wellness, 23-36. https://doi.org/10.1016/B978-0-12-818309-0.00006-X
- Electrocauterization: MedlinePlus Medical Encyclopedia. (n.d.). https://medlineplus.gov/ency/article/002359.htm













